Tissue engineering is a set of biotechnological approaches aimed at reproducing outside the biological organism the structures and functions of tissues and organs using various tools. One of them is the cultivation of cells, often not only in so-called culture dishes (as is done for other biotechnological purposes), but in three-dimensional structures created from elements of the extracellular matrix or similar substances. Such structures can be printed on a 3D printer or created in another way. We often hear the expression “growing organs “, but it is worth emphasizing that the process of engineering tissue structures is very complex, so the word “growing” is not quite adequate to describe it. However, there is still no other term that would be just as convenient to use in everyday life, so we will try to draw some parallels with growing plants in the garden.
As of May 21, 2019, 571 people have traveled into space. And every day we hear more and more about the development of biotechnology in extraterrestrial conditions and the prospects of staying on other planets.
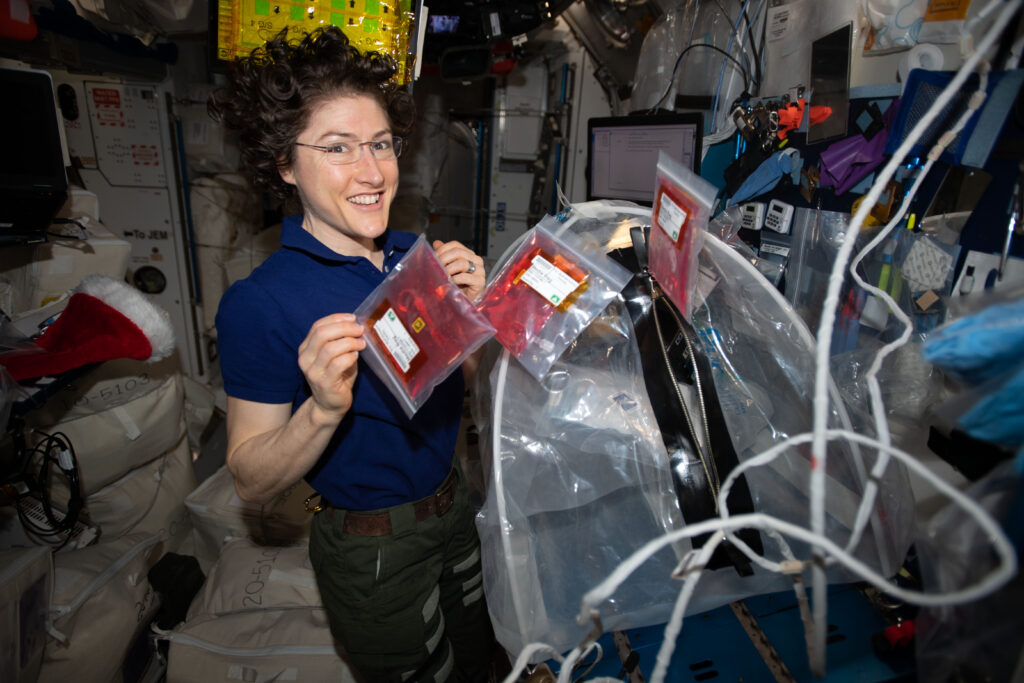
On Earth, the force of gravity is constant, and although its exact magnitude depends on location, the standard value of the acceleration due to Earth’s gravity is 9.81 m/s2. On the International Space Station (ISS), astronauts are in a state of free fall, since any spacecraft in Earth orbit must move at such a speed that its deviation from a straight line due to gravitational acceleration corresponds to the curvature of the planet’s surface (more precisely, the curvature of orbit at the corresponding altitude). Thanks to this, the forces acting on all objects and crew members of the orbital complex are millions of times smaller than in terrestrial conditions. This state is called weightlessness or, more precisely, microgravity. It is ideal for studying the effect of the absence of gravity on living systems, including studying their growth and development both at the cellular level (in cell culture) and in complex systems where different new approaches may be needed to build tissue architecture, including additional frames. But there are already data on certain advantages of working with cells in microgravity conditions. Thus, it turned out that stem cells in such conditions show this stemness more vividly, and some cells that have already managed to “choose their fate” (specialization), can even dedifferentiate — that is, “roll back to previous settings”.
The word “growing” has several associations. For instance, we usually need seeds to grow some vegetable. In tissue engineering, seeds are replaced by cells. Both stem and specialized cells can be used for this work. The former are the topic of a separate article, because they are divided into several types with fundamentally different properties and potential gamma of transformations. The main thing that distinguishes a stem cell from a specialized “workhorse” is the ability to transform into other types of cells and to divide asymmetrically (that is, to produce not two identical cells during division, but one differentiated cell and one stem cell).
Developing our “agro-comparison”, the seed must be planted in a certain soil. This function in tissue engineering is performed by various matrices and frameworks. Today, scientists have access to a huge number of materials for such structures. These are synthetic, natural, biodegradable (that is, those that dissolve themselves over time after entering a living organism) and stable. Depending on the task, sometimes it is necessary that the material only gives the structure a certain shape and gives the opportunity for the cells to be located optimally, and then it is more expedient for it to disappear without harm. Sometimes it is desirable that it remains in the body for a long time and stays intact. But simply throwing a seed into the ground does not guarantee producing of a viable plant. The soil needs to be fertilized. To create a tissue-engineering structure, it is necessary to control the factors that cause the stem cell to turn into a specific type of cells planned for this particular place. Therefore, during work, various inducing factors are used — cytokines, hormones, complex cocktails of substances that send a signal to the cells that this particular tissue should be formed right here and right now. Also, of course, all described processes require control. Such works require incredibly expensive equipment and have very high requirements for safety and cleanliness.
Organoids are an extremely important object of research for fundamental biology and medicine. Basically, these are microscopic or very small areas of a certain organ, formed by several types of cells in the culture. Such “balls” or “plates” of cells are used to study those processes that occur during the formation of a certain tissue or organ, allow to investigate complex intercellular interactions and the influence of various factors on the formation of specific structures. With the help of organoids, it is possible to understand how an organ develops during embryogenesis or how it regenerates when needed. Also they can be used to simulate various pathological processes. After all, understanding how everything happens can help find “targets” for treatment. It is also important to be able to influence the “sick” organoid with various substances and test the expediency of their use in simulated pathologies. Unfortunately, very often the work with organoids is mistaken for “growing organs” by the unqualified mass media. Recently, one laboratory was able to create an organoid to study the course of neurodegenerative diseases, and it was already loudly called “an adult brain in a test tube.”
Another well-known trend is 3D printing. We often hear about “printed organs”, and this also needs clarifying. With the help of a 3D printer, you can create frameworks and matrices for tissue engineering structures. To do this, the shape of the desired organ is modeled using some biocompatible material, and the necessary “blank” is formed. In some cases, to restore the structure, it is enough to replace the lost part with such a fragment, and over time, the organism’s own cells will “feel at home” with it. In such a way scientists managed to restore nose and ears. Sometimes the printed form is additionally filled with stem cells and we wait for successful “inhabitation” and transformation into the desired tissue composition under the influence of inducing factors. In these cases, we are talking about printing an exclusively “inanimate” component, and such operations are already quite widespread in the field of regenerative medicine. Another approach is actual “bioprinting” — when a structure is formed by a 3D printer, in which the role of “ink” is played by living cells. In this regard, there are a number of skeptical comments, because the conditions under which the printing process takes place are not entirely acceptable for maintaining the viability of cells. Today, only mini-copies of organs are “printed”, which can be useful for basic science and modeling of certain conditions, but not for transplantation into humans. However, in 2019, it was on board the ISS that an important step was taken in bioprinting in microgravity — fragments of a mouse thyroid gland were “printed”. Further research in this direction is actively ongoing.

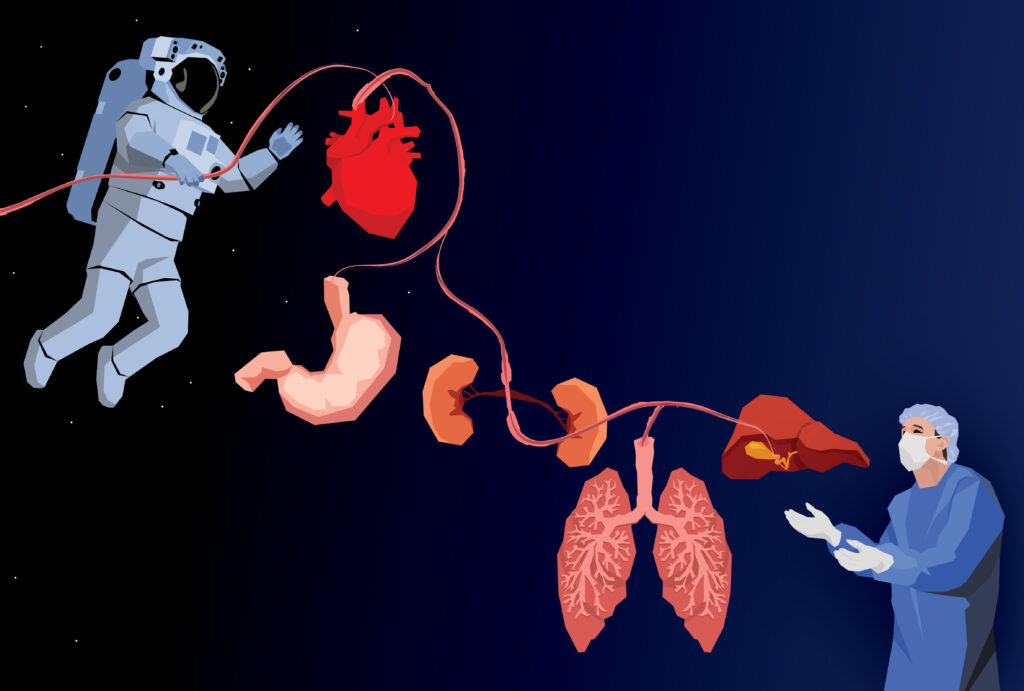
It should be noted that all successes in the creation of organs outside the body are limited only to the possibility of reproducing a fragment of a full-fledged organ (intestine, liver, etc.), and not to create a completely autonomous organ, which, like in a fantastic movie, can simply be brought to the operating room on a plate. If with hollow structures consisting of several types of cells, such as the urinary bladder, or with cartilage, the situation seems optimistic and we can really hope for the rapid introduction into routine practice of methods of their replacement, then with complex organs consisting of many layers and having a specific architecture, everything is not so simple. In this area, there are several stumbling blocks for modern tissue engineering. The first is vascularization, that is, penetration of blood vessels. This is a significant problem, but little by little it is being solved by combining cell types and introducing precursors of blood vessel-forming cells. The most original method was described a few years ago: the vascular system of plants was used for vascularization — literally, cardiomyocytes (heart cells) were grown on prepared spinach leaves with developed veins. Most likely, the issue of vascularization of newly formed organs will be resolved earlier than others.
The second problem is innervation, that is, the penetration of nerve endings into the organ. Everything is more complicated here, but there are also positive developments. The third question, the solution of which is the subject of the most heated discussions, concerns the central regulation of the activities of each of our organs. When we are formed from two cells and continue to develop throughout our lives, all processes are regulated on several levels, the main of which is neurohumoral, that is, related to the nervous system and hormones. Cells “communicate” with each other by chemical and electrical signals, each organ knows why it is located here and is in this state, what it should do and what signals to transmit to other structures. Everything is intertwined on many levels of understanding. And if the immune issue of ” friend-or-foe” identification can be solved simply by taking one’s own cells to create an organ (admittedly, this is also not always possible, but there are approaches using cells that do not carry markers of the immune response, so this issue can also be considered at least partially solvable), then the method of introducing a new component, which was created outside the competence of the neurohumoral regulator of a particular organism, into an extremely delicate and interwoven system of interactions is much more complicated. In fact, creating even an ideal organ in the laboratory does not guarantee its unquestionable “acceptance into the family” by the organism as a whole. It is possible that research in microgravity — real in space or artificially created in special laboratories on airplanes — will make it possible to take a key step in overcoming at least some of the problems arising in the field of tissue engineering today.
As a part of discussion about all these questions, a 2016 review in the Nature journal made an assumption regarding the further development of cell engineering: either we continue to follow the same paths and wait for the development of existing technologies (bioprinting, tissue building out of stem cells, etc.), or already in the near future a certain revolutionary technology will appear, which will probably be strategically different from the currently known approaches. A 2019 review by the same authors notes that tissue engineering is becoming increasingly closer to the clinic (including due to changes in regulatory approaches), but still remains largely experimental rather than routine. Meanwhile, of course, the introduction of all these results into medical practice is only a matter of time.

